Abstract
Introduction/Background:
There are no evidence-based guidelines for optimal transfusion practices for patients undergoing chemotherapy and stem cell transplant. There are minimal low-quality studies regarding transfusion thresholds as well as the efficacy of pre-transfusion medications (to reduce febrile non-hemolytic transfusion reactions) for these patients. To pursue a prospective quality improvement study, it is important to know the current transfusion standards used by practitioners regarding: 1) transfusion thresholds for platelets and red blood cells and 2) routine use of pre medications prior to transfusions. Additional research questions included differences in the above standards by region or by pediatrics vs. adult providers.
Study Design and Methods:
Expedited IRB approval was obtained. We conducted a REDCap survey from 3/1/18-4/12/18 targeting hematology oncology providers of both pediatric and adult providers. The survey was emailed through multiple databases with members form several countries that included both adult and pediatric hematology/oncology practitioners.
Results:
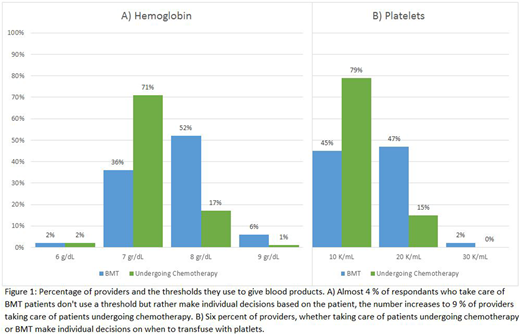
One hundred and nineteen hematology/oncology practitioners completed the survey: 94 attending physicians, 19 fellows and 6 nurse practitioners. Most respondents practiced in United States (90 %, 107/119), the rest practiced in Canada, India, Italy and Iran. The majority of participants were pediatric hematology/oncology providers (84 %, 100/119). Of the remaining providers 10 treated only adults and 9 treated both adults and children. The vast majority (97%, 115/119) of participants did not utilize a standard policy for premedication prior to red blood cell transfusions. Similarly, 95 % (111/117) or participants made individual decisions on premedication with platelet transfusions rather than using an institutional policy. When asked about the threshold to transfuse blood products, 71% (75/105) of those who treated patients undergoing chemotherapy said they would transfuse red blood cells when patients had a hemoglobin of</= 7 g/dL, and 79% (82/104) would transfuse platelets when patients had a platelet count <10 K/mL. Practitioners treating bone marrow transplant (BMT) patients had more variability and used higher transfusion thresholds. Fifty-two percent (33/64) of them would transfuse red blood cells for patients undergoing BMT with a higher threshold of hemoglobin of 8 g/dL while only 36% used the lower threshold of 7 g/dL. Similarly, for platelet transfusions for patients undergoing BMT, 47% (31/66) would use a 20K/mL threshold, and 45% would transfuse platelets at a threshold of 10 K/mL.
Conclusion:
There is currently no routine practice of utilizing pre-medications prior to transfusions of red blood cells or platelets. Instead, practitioners surveyed indicated a preference for individualizing the use of pre-medications only if patients had a previous transfusion reaction. As the use of these medications is not evidence-based, additional studies are needed to determine their efficacy. Transfusion thresholds are relatively consistent among providers with the majority aiming for more liberal thresholds in patients undergoing chemotherapy and more conservative for those undergoing BMT. More studies are needed to evaluate the risks and benefits of using different transfusion thresholds.
Kanter:Sancilio: Research Funding; ASH: Membership on an entity's Board of Directors or advisory committees; NHLBI: Membership on an entity's Board of Directors or advisory committees, Research Funding; bluebird bio: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Global Blood Therapeutics: Research Funding; Apopharma: Research Funding; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.